
To account for differences in disease burden among the patient population of Medicare Advantage (MA) plans, risk adjustment based on the patient’s disease burden is used. Specifically, MedPAC notes that:
Medicare uses beneficiary characteristics, such as age and prior health conditions, and a risk adjustment model (the CMS Hierarchical Condition Categories (CMS-HCC)) to develop a measure of your expected relative risk for Medicare-covered spending.
In February 2023, CMS CMS published a notice of proposed rulemaking to update its HCC risk adjustment algorithm (v28). These changes included (i) leveraging ICD-10 codes instead of ICD-9 codes as principal components, (ii) using 115 HCC indicators instead of 79, and (iii) restricting some coefficients. so that they are identical at all levels of severity (e.g., diabetes, heart failure). The new algorithm will be implemented gradually between 2024 and 2026.
A key question is whether providers under the traditional Medicare (TM) code are different than Medicare Advantage (MA) plans. Because MA plan payment by CMS depends on patient acuity, there is an incentive to code diagnoses. An article by Carlin et al. (2024) aims to evaluate whether this occurs or not. They first explain the mechanism through which MA plans could more completely capture patients’ secondary diagnoses:
MA plans have the opportunity to review medical records to ensure that providers do not accidentally omit a diagnosis from encounter records. These reviews are most important when provider reimbursement does not incentivize detailed coding of patients’ secondary diagnoses. MA plans to make corrections to add or (rarely) remove a diagnosis through CR records. Additionally, both MA and TM providers can record additional diagnoses through an HRA. [health risk assessment] during a wellness visit or a home visit for this purpose.
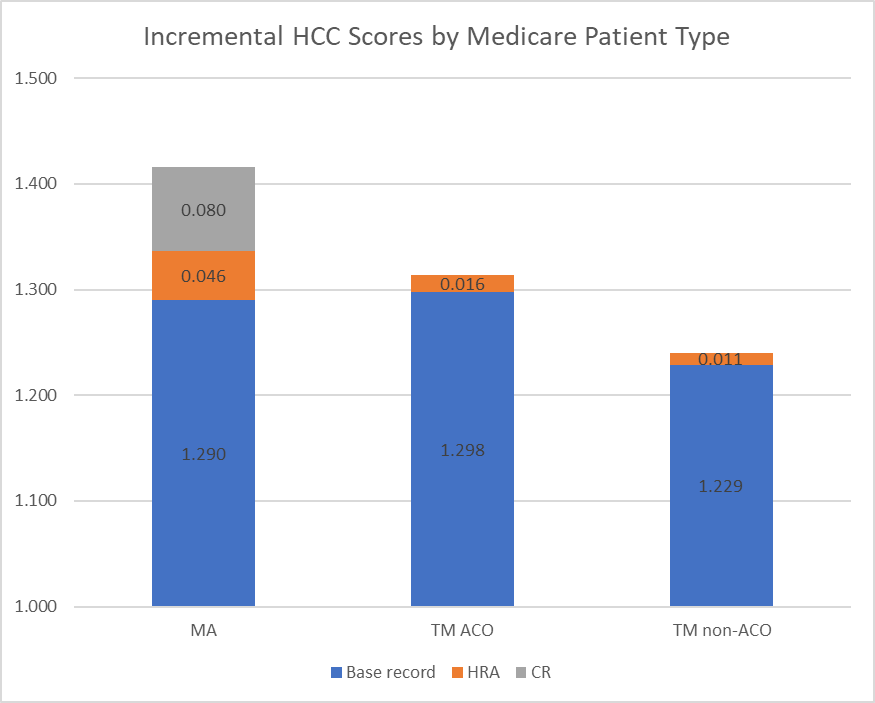
The authors use 2019 CMS claims data and divide the data into 3 cohorts: MA plans, TM beneficiaries attributed to ACOs (“TM ACOs”), and TM beneficiaries not attributed to an ACO (“TM non-ACOs”). ACOs include patients attributable to accountable care organizations (ACOs), such as those participating in the Medicare Shared Savings Program (MSSP). The authors note that the non-ACO TM cohort serves as a key comparison, as they are not subject to the same coding intensity incentives that MA plans and TM ACOs experience (given ACOs’ shared savings are also risk-adjusted).
The authors identify patients who had an HRA based on whether they had an annual wellness visit, an initial preventive physical exam, or selected home health visits (after Reid et al. 2020 algorithm). The authors also use information from encounter statements about whether a review of the patient’s record was performed. Using these data, the authors propensity score matched the MA, TM ACO, and TM non-ACO cohorts. The authors then compared matched and unmatched HCC scores and assessed how HRA and CR visits impacted HCC risk scores. They find:
Incremental health risk due to diagnoses in HRA records increased across all coverage cohorts in line with incentives to maximize risk scores: +0.9% for non-ACO TM, +1.2% for TM ACO and +3.6% for MA. Including the HRA and CR registries, MA risk scores increased by 9.8% in the matched cohort.
Diagnosis codes related to vascular conditions, congestive heart failure, and diabetes had the largest contribution to the average HCC score in the 3 cohorts. Vascular, pscyh, and congestive heart failure were more likely to increase due to HRA/CR coding intensity activities.
While other articles have claimed that Medicare Advantage has downcoded diagnoses to obtain more favorable reimbursement, this article clearly specifies not only the magnitude of the impact, but also the mechanism through which it is most likely to occur. You can read the full article. here.







