
See my previous posts on negotiating IRA prices in drug selection (Part 1) and sending manufacturer data (Part 2).
Today we will talk about the negotiation process and how CMS will set the maximum fair price (MFP)
How will CMS be priced across all doses?
“CMS will base the single price on the cost of the selected drug per 30-day equivalent supply (rather than per unit, such as tablet, capsule, injection, or by volume or weight-based metric), weighted between dosage forms and strengths. .”
Is there a maximum value or “ceiling” for the maximum fair price (MFP) that CMS will offer?
The maximum amount of the MFP will not exceed:
- An amount equal to the sum of the plan-specific weighted enrollment amounts
- The lower of: the average non-FAMP price in 2021 increased by inflation (IPC-U) or the average non-FAMP price in February 2025
CMS will aggregate the 60 quantities determined for each NDC-11 for the selected drug to calculate a single quantity (separately for each methodology) across all dosage forms, strengths, and package sizes of the selected drug. These quantities can then be compared directly and the maximum limit for the single MFP of the selected drug (including all dosage forms and strengths) will be the lowest quantity.
Sample packs, NDCs from secondary manufacturers, NDCs with no dispensed quantity, or NDCs with $0 gross covered prescription drug costs will not be included in the MFP calculation.
Can some claims be excluded from the MFP refund?
Once the price of the MFP is determined, there are some cases where a manufacturer would not have to pay the MFP rebate. These include:
“…[justification] codes for the drug that is prospectively purchased at or below the MFP, the manufacturer and dispensing entity have a separately negotiated reimbursement amount other than the Default Standard Reimbursement Amount, and the claim is excluded from MFP reimbursements under Sec. 1193(d)(1) of the act”
CMS has to justify the MFP to manufacturers. How will you do this?
The CMS justification will follow a 4-step process:
- Identification of therapeutic alternatives, if any, for the selected medication.. This includes drugs approved by the FDA for the relevant indication and off-label use if they are included in nationally recognized, evidence-based guidelines and a CMS-recognized compendium. CMS will begin by identifying therapeutic alternatives within the same pharmacological class as the selected drug based on properties such as chemical class, therapeutic class, or mechanism of action, and will then also consider therapeutic alternatives in different pharmacological classes based on CMS’s review of relevant data. . (see question below).
- Measure the price of therapeutic alternatives. For Part D drugs, this is the total gross covered drug cost (TGCDC) net of DIR and CGDP payments and/or the average sales price (ASP) for Part B drugs (or the MFP from the previous year, if applicable).
- Determine if the medication has a unique benefit. To evaluate whether the selected medication, relative to therapeutic alternatives, addresses an unmet need, has a beneficial impact on specific ARI populations, and to what extent the selected medication represents a therapeutic advance compared to therapeutic alternatives.
- Further preliminary price adjustment. These adjustments will be based on data submitted by the manufacturer, including: (1) R&D costs and recovered R&D costs, (2) current unit costs of production and distribution; (3) prior federal financial support for the discovery and development of new therapies; (4) pending and approved patent applications or exclusivities; and (5) market data and U.S. drug sales volume and revenue data, and (6) optional data submitted by the manufacturer.
What data does CMS use to determine therapeutic alternatives?
“…CMS will use data submitted by the primary manufacturer and the public, FDA-approved indications, drug classification systems commonly used in the public and commercial sector for formulary development, CMS-recognized Part D compendiums, clinical guidelines widely accepted, led by CMS. literature review, reviews of drugs or drug classes, and peer-reviewed studies.”
How could CMS set the initial price offer?
The primary way CMS will set its initial price offering for 2027 is based on the net price of therapeutic alternatives.
However…
If the selected medication has no therapeutic alternative, if the prices of all identified therapeutic alternatives are above the legal limit for the MFP… or if there is only one therapeutic alternative for the selected medication and its price is above the legal limit for the MFP will then determine the starting point for the initial offer based on the FSS or… the “Big Four price”… whichever is lower. If the FSS and Big Four prices are above the legal ceiling, then CMS will use the legal ceiling as a starting point for the initial bid.
Why did CMS decide to set its initial price based on the price of therapeutic alternatives?
Please note that CMS considered a variety of options to establish the initial price offer, including net prices, unit production/distribution cost, national reference price at the Federal Supply Schedule (FSS) price, a “fair profit” price ” based on whether R&D costs have been recovered and margins have been obtained on the unit costs of production and distribution, but have been settled on the net price of therapeutic alternatives.
However, he maintains that the net price of therapeutic alternatives—despite limitations—is a preferred option:
“In taking this approach, CMS recognizes that the price of therapeutic alternatives for a selected drug may not reflect its clinical benefit; however, the use of Part D Plan Net Payment and Beneficiary Responsibility, ASP, or MFP for therapeutic alternatives allows CMS to begin developing the initial offering within the context of the cost and clinical benefit of one or more drugs that treat the same disease or condition. When using the prices of therapeutic alternatives for the selected drug, CMS may focus the initial offer on the section 1194(e)(2) factors by adjusting this starting point in relation to whether the selected drug offers more, less, or similar benefit. compared to its therapeutic alternative(s).”
What factors will affect CMS’s decision to adjust its initial offer?
Some considerations include:
- Clinical benefit conferred by the selected drug in comparison with its therapeutic alternative(s),
- Impact on patient-reported outcomes and patient experience
- Impact on caregivers
- Patterns of use of the selected drug versus its therapeutic alternative(s)
- Feedback from consultations with physicians, patients or patient organizations, academic experts, and/or the FDA
- Impact on CMS Special Populations (Individuals with Disabilities, the Elderly, the Terminally Ill, Children, and Other Medicare Beneficiaries)
- Whether or not the treatment meets an unmet medical need
Key relevant information that will be considered includes: “…peer-reviewed research, expert reports or technical papers, clinician experience, real-world evidence, and patient experience.” Key outcomes of interest to consider include a variety of outcomes, including patient-centered outcomes and patient experience.
Although CMS notes that it will not use QALY-based cost-effectiveness analyses, it has not ruled on whether it may use other approaches such as equal value of life years gained (evLYG), health years in total (HYT), or generalized and risk. -Adjusted QALY (GRA-QALY).
These factors will affect the price through a qualitative decision process.
Will caregiver experience affect CMS decisions?
Yeah. The guidance says that “CMS may also consider the caregiver’s perspective to the extent it directly reflects the relevant experience or outcomes of the patient taking the selected medication.”
Does CMS consider cost when evaluating whether a treatment is a therapeutic advance?
Yeah.
“CMS will determine the extent to which a selected drug represents a therapeutic advance compared to its therapeutic alternative(s) by examining improvements in outcomes compared to its therapeutic alternative(s). (for example, the selected medication is curative versus a therapeutic alternative that delays progression) and will consider the costs of said therapeutic alternatives. CMS may consider a selected drug to represent a therapeutic advance if evidence indicates that the selected drug represents a substantial improvement in outcomes compared to therapeutic alternatives of the selected drug for an indication.”
How will the negotiation process work?
This is summarized in the following graph.
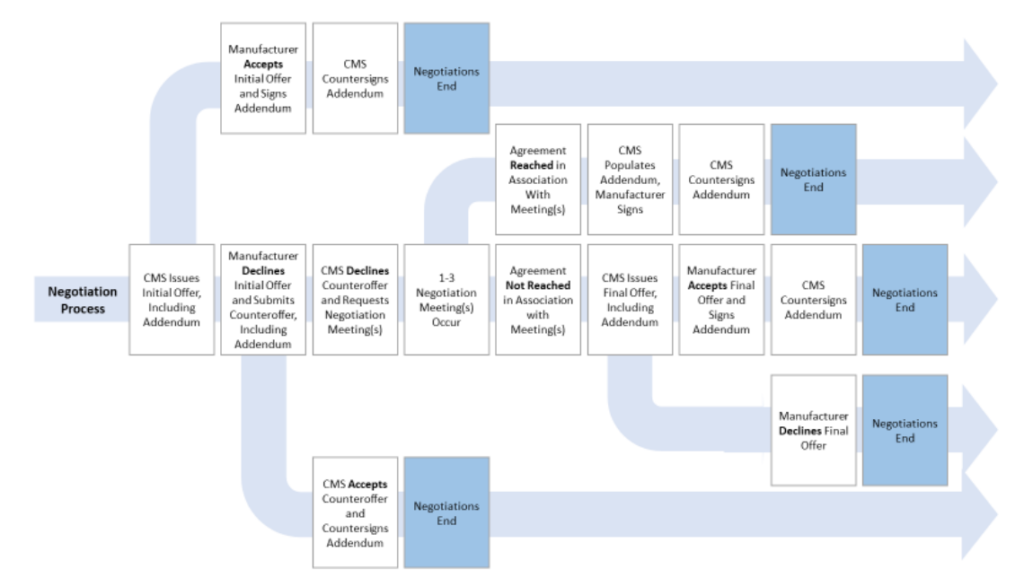
More details can be found in the CMS guidance document. here.







