One reason is that Medicaid reimbursement rates are lower than those of Medicare or commercial insurance. However, another (often overlooked) factor is the risk of doctors being denied payments and the administrative problems they face when trying to obtain reimbursement from Medicaid. an article of Dunn et al. (2024)–cleverly named “One denial a day keeps the doctor away“–shows that Medicaid reimbursement denials are much higher than those from Medicare or commercial insurance.
Who bears the consequences of administrative problems in health care? We use data on repeated interactions between a large sample of US physicians and many different insurers to document the complexity of health care billing and estimate its economic costs to physicians and consequences for patients. By observing the back-and-forth sequences of claim denials and resubmissions from previous visits, we can estimate doctors’ costs in haggling with insurers to collect payments. Combining these costs with revenue never collected, we estimate that physicians lose 18% of Medicaid revenue due to billing problems, compared to 4.7% for Medicare and 2.4% for commercial insurers. By identifying physician moves and practices that span state lines, we find that physicians respond to billing problems by refusing to accept Medicaid patients in states with more severe billing barriers. These barriers are quantitatively as important as payment rates in explaining variation in physicians’ willingness to treat Medicaid patients. We conclude that administrative frictions have first-order costs for physicians, patients, and equality of access to health care. We quantified the potential economic gains (in terms of reduced public spending or increased access to doctors) if these frictions could be reduced and found them to be considerable.
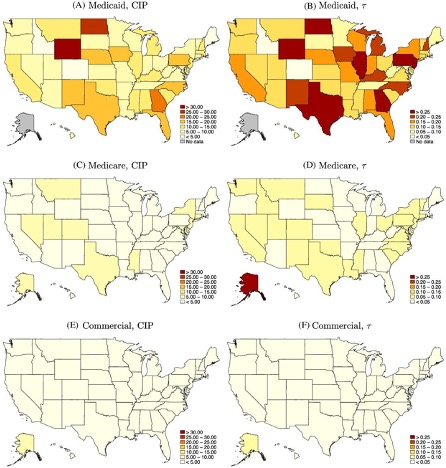
The right column shows the mean CIP as a percentage of visit value by state and payer.“
Economist writing every day It has a good summary of the problem.








