
 Introduction
Introduction
Children with non-ambulatory cerebral palsy (CP) at GMFCS levels IV and V have limited opportunities for independent mobility; This predisposes them to the effects of immobility and progressive secondary deformities such as postural asymmetries. Research supports postural management at the amber or “probably will” level, meaning that the evidence is low quality and a good outcome measure is needed to assess the effectiveness of the intervention.
A recent paper by Paleg and colleagues, titled Evidence-based clinical perspectives on postural management for hip health in children and adults with non-ambulatory cerebral palsyprovides information on current postural management guidelines for supported lying, sitting, and standing, as well as supported stepping and orthotics.1 The article examines the available evidence to synthesize recommendations throughout the lifespan, based on the ICF model and “F-words” framework: Fitness (body structure and function), Function (activity), Friends (participation), Family (environmental factors), Fun (personal factors) and Future.2 Emphasizing the F-word taxonomy allows clinicians and caregivers to focus more on the environment, family needs, and patient involvement than on specific body structures and functions while developing goals.
Considerations for Lying and Night Positioning Support
Regarding postural supports while lying and sleeping, the article discusses the effects of supported sleep in decreasing the incidence of pain, reducing the risk of windswept deformities and hip dislocations, and improving comfort and quality of the dream. The authors note that patients who cannot change their sleeping position are more likely to have postural asymmetries, especially if the static position persists for more than eight hours. This may be particularly poignant for people classified as GMFCS levels IV and V, where tolerance for multiple sleeping positions is low. The existing body of evidence, although minimal, points to the general benefits of nocturnal postural management in children with cerebral palsy, while recognizing that sleep disturbances and discomfort make compliance with protocols difficult in some cases. So, when considering postural support for the prevention of musculoskeletal asymmetries, considerations of sleep quality and pain reduction in these positions are of equal importance. Therefore, children with non-ambulatory cerebral palsy require comprehensive and regular postural assessment, incorporating family information to determine appropriate positioning systems and lying positions to achieve the best results.
Considerations for adaptive seating
Adaptive seating has broad support through consensus clinical practice, with no evidence of harm to the intervention found. The authors summarize available research indicating that upright positioning in an adaptive chair can potentially increase activity and participation levels, upper extremity function, lung function, and reduce blood pressure. In particular, contoured seats or lateral and pelvic supports that increase hip abduction may decrease windswept positions and increase sitting tolerance. Additionally, the authors note that although there is limited evidence regarding supported seating and its effect on hip stability, positioning intervention is still believed to slow the progression of hip deformity. And despite continued discrepancy in the literature, clinical practice suggests that 10 to 15 degrees of hip abduction is well tolerated in sitting and is said to reduce the negative effects of spasticity, further underscoring the importance of adaptive sitting as part of a comprehensive postural strategy. management plan.
Considerations for supported standing and weight bearing
It is generally recognized that supported weight bearing while standing in children with motor disabilities increases bone mineral density, improves range of motion and hip stability, but high-quality evidence supporting these recommendations remains lacking. . The authors note that studies recommend standing with hip abduction of between ten and fifteen degrees, as this appears to be more tolerable for children with spasticity. The recommended dose to stop the rate of hip migration is believed to be at least one hour five times a week, and the intervention is continued for years to maintain optimal hip stability. Additionally, standing allows individuals to participate more during ADLs and activities with peers.
Supported steps with a gait trainer increase physical activity and improve walking ability. To date, there are no studies demonstrating the impact of supported stepping on hip stability, but bone mineral density and joint development are thought to improve with gait training.
Clinical recommendations
The review article concluded by making seven clinical recommendations on how to apply the evidence on positioning and postural management for children functioning at GMFCS levels IV or V.
- Comfortable and non-injurious sitting and lying positions should be promoted and, if possible, the possibility of adopting one or more sleeping positions is also beneficial. Medial thigh support when lying down and the use of a molded seat or abductor should be used to prevent hip adduction and windage in children with increased tone. Frog-leg positions (excessive bilateral hip abduction, flexion, and external rotation) can be avoided by using full lateral support of the pelvis and thighs in children with decreased tone.
- Supported standing should be encouraged for at least one hour daily in 10 to 15 degrees of bilateral hip abduction.
- All positioning and supporting equipment or devices are to promote functioning and greater participation in activities.
- Movement and active weight bearing using a supported stepping device reduces sedentary behavior, as well as other activities such as cycling and swimming.
- Unsupported supine position should be avoided, especially during the day, increasing time in various upright positions. No position should be held for more than eight hours.
- Postural management is important during all parts of the daily routine and should be considered during transfers, feeding, toileting, dressing, and bathing. Figure 1 below outlines the appropriate age for the introduction of these interventions.
- A valid and reliable postural assessment should be used to identify problems and intervene early.
Conclusion
Overall, it is very important that when implementing these postural recommendations, a client-centered team approach is adopted so that individual preferences and goals are taken into account. The ICF and F-word frameworks provide useful guidelines to ensure that chosen interventions improve patient participation and activity, as well as maximize independence to facilitate care delivery.
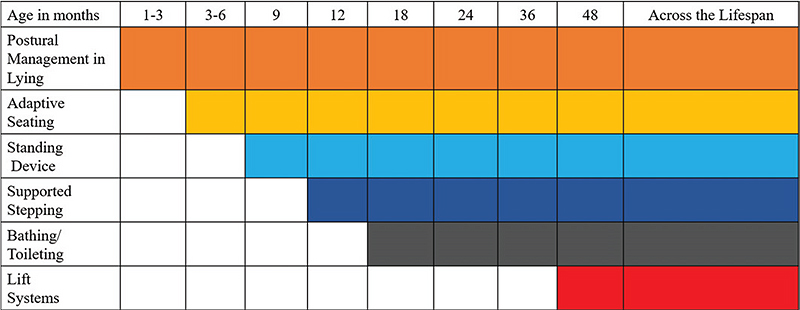
Figure 1







