that is the answer Caswell-Jin et al. (2024) objective to respond. The authors used 4 cancer mortality models within CISNET for this study:
- Model D (Dana-Farber Cancer Institute). It is used to define a set of disease states and analytical formulations implemented to estimate the association of interventions on transitions between these states, as well as on breast cancer incidence and mortality.
- Model M (MD Anderson Cancer Center). It was based on a Bayesian approach, which evaluated the probability distributions of unknown parameters, including treatment benefits, and adjusted for observed breast cancer mortality.
- model S (Stanford University). A microsimulation that modeled the natural history of the disease based on tumor size and stage progression mapped to detection; The benefits of the treatments were applied to the initial survival curves according to stage, age and estrogen receptor (ER)/ERBB2 (before HER2) state at the time of detection.
- model W (University of Wisconsin-Harvard). This model used a tumor growth framework and calibrated incidence and mortality according to the Surveillance, Epidemiology and End Results (SEER) Program registry. This model also incorporated a curing fraction.
Categories of breast cancer by RE/ERBB2 status (ER+/ERBB2-, Emergencies+/ERBB2+, emergency room−/ERBB2+ and emergency room−/ERBB2-) were modeled separately.
Using this approach, the authors found that:
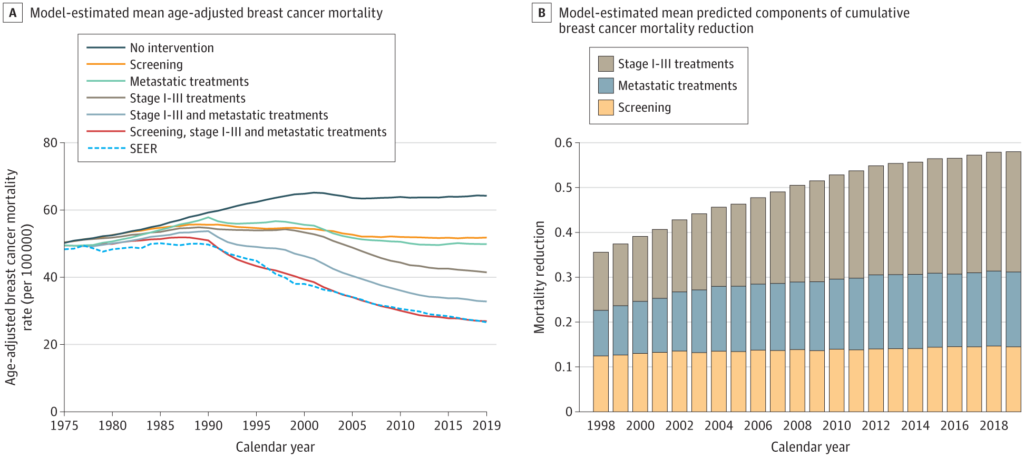
The breast cancer mortality rate in the US (age-adjusted) was 48/100,000 women in 1975 and 27/100,000 women in 2019. In 2019, the combination of screening, stage I treatment a III and metastatic treatment was associated with a 58% (model range, 55%-61%) reduction in breast cancer mortality. Of this reduction, 29% (model range, 19%-33%) was associated with treatment of metastatic breast cancer, 47% (model range, 35%-60%) with treatment of early-stage breast cancer. I to III, and 25% (model range, 21%-33%) with screening mammography. Based on the simulations, the largest change in survival after metastatic recurrence occurred between 2000 and 2019, from 1.9 years (model range, 1.0 to 2.7 years) to 3.2 years (model range , 2.0 to 4.9 years).
You can read the full article. here.








